Disease X
placeholder name that was adopted by the World Health Organization (WHO) in February 2018 on a shortlist of blueprint priority diseases to represent a hypothetical, unknown pathogen that could cause a future epidemic
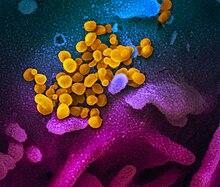
Disease X is a placeholder name that was adopted by the World Health Organization (WHO) in February 2018 on their shortlist of blueprint priority diseases to represent a hypothetical, unknown pathogen that could cause a future epidemic.
Quotes
edit- The scale of the plague is surprising, indeed shocking, but not its appearance. Nor the fact that the U.S. has the worst record in responding to the crisis. Scientists have been warning of a pandemic for years, insistently so since the SARS epidemic of 2003, also caused by a coronavirus, for which vaccines were developed but did not proceed beyond the pre-clinical level. That was the time to begin to put in place rapid-response systems in preparation for an outbreak and to set aside spare capacity that would be needed. Initiatives could also have been undertaken to develop defenses and modes of treatment for a likely recurrence with a related virus. But scientific understanding is not enough. There has to be someone to pick up the ball and run with it. That option was barred by the pathology of the contemporary socioeconomic order. Market signals were clear: There’s no profit in preventing a future catastrophe.
- Noam Chomsky in an interview with C.J. Polychroniou, "Chomsky: Ventilator Shortage Exposes the Cruelty of Neoliberal Capitalism", Truthout (April 1, 2020)
See also
editExternal links
edit